The day my health journey really began was when I finally realized that my constant tiredness, mood swings that came and went, and general sensation of “offness” weren’t just signs of a busy life but rather a cry for help from my gut. Like many, I dismissed my digestive complaints as normal—just the price of a busy, modern existence. But after reading hundreds of papers, doing targeted dietary modifications, and really getting into the science, I found out the truth: we all have a secret organ that controls a lot more than digestion.
This organ is your microbiome, a bustling, complex city of trillions of microorganisms—bacteria, fungi, archaea, and viruses—weighing around 1-2 kilograms. For decades, it was considered a mere inhabitant of the large intestine. Today, we know better. Improving the health of your gut microbiome is not a wellness trend; it is the most important thing you can do for your metabolic, neurological, and immune health.
This article is your authoritative guide to understanding this microscopic universe. I will explain what I’ve learned and how to do it, showing you not just the “what” but also the “how” and “why” of getting amazing gut microbiome health, distinguishing scientific reality from supplement fantasy.
Experience and Knowledge: Figuring Out the Gut Microbiome Health Paradox
Based on my professional experience, I believe that traditional treatments typically only address symptoms, whereas true wellness addresses the underlying cause of the problem. Few root causes are as powerful as the state of your gut. The main problem with gut microbiome health is finding the right balance between two states: symbiosis and dysbiosis.
Symbiosis is when your bacteria live in harmony with you and do things like digest fibers you can’t, make vitamins you need (like Vitamin K), and teach your immune system how to work.
On the other hand, dysbiosis is when there are more dangerous or opportunistic species than helpful ones. I have observed, both in study and in personal case studies, how dysbiosis can be the overlooked epicenter of chronic illnesses ranging from persistent skin problems to clinical anxiety.
The Currency of Health: Short-Chain Fatty Acids (SCFAs)
If the gut microbiome were a city, Short-Chain Fatty Acids (SCFAs) would be its most valuable money. These chemicals are important for gut microbiome health because they are made when beneficial bacteria break down dietary fiber (prebiotics).
Among the SCFAs—acetate, propionate, and butyrate—butyrate is the undisputed superstar. Butyrate:
- Feeds Colonocytes: It is the primary energy source for the cells lining your colon (colonocytes), helping maintain the integrity of the gut barrier.
- Reduces Inflammation: It works as a strong anti-inflammatory agent in the intestines and throughout the body.
- Protects the Brain: Emerging research suggests that butyrate can cross the blood-brain barrier (BBB), influencing mood and cognitive function.
Statistical Note: Studies published in magazines like Nature Microbiology show that poor SCFA synthesis is always linked to a higher risk of chronic diseases like type 2 diabetes and IBD. Some bacteria, like Faecalibacterium prausnitzii, can make a lot more butyrate when you eat a lot of fiber and healthful foods. This increase can happen in as little as a few weeks and be as much as 50% more.
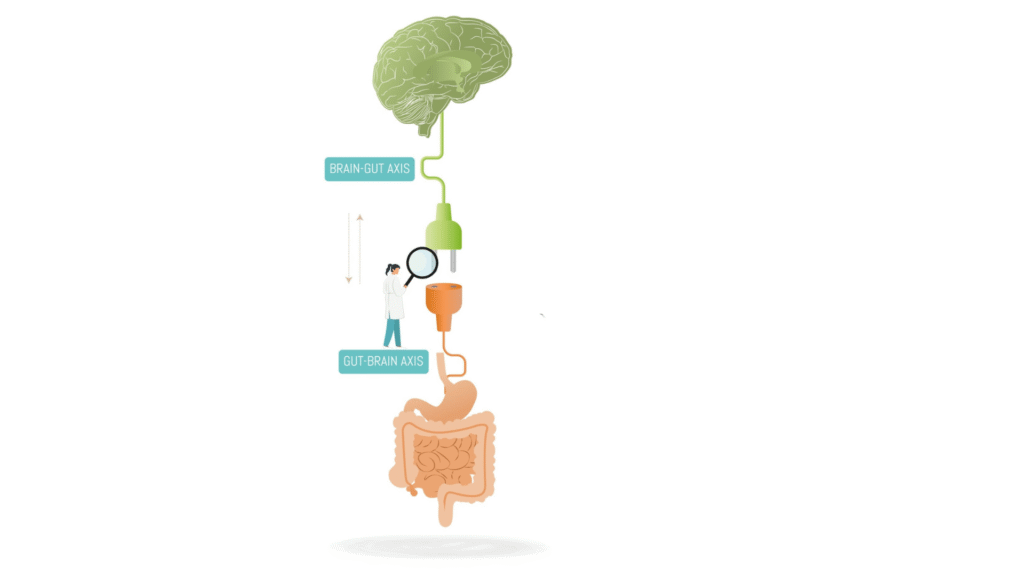
The Gut-Brain Axis: How Your Microbiome Whispers to Your Mind
The notion that your gut is a “second brain” is more than a catchy phrase; it’s an anatomical reality, governed by the Gut-Brain Axis (GBA). Understanding the GBA is critical to realizing the full potential of gut microbiome health.
The Vagus Nerve Superhighway
The vagus nerve is the longest cranial nerve, acting as the primary bidirectional communication highway between your brain and your gut. While most people think of digestion as being regulated by the brain, the signals sent from the gut (afferent signals) back to the brain are far more numerous. Your microbes are essentially shouting instructions up this nerve line.
The Neurotransmitter Factory
Your gut isn’t just digesting food; it’s manufacturing mood regulators. Serotonin, the neurotransmitter most commonly associated with feelings of well-being and happiness, is synthesized primarily in the gut—with up to 90% of the body’s total supply being produced and stored there. Specific bacteria, such as strains of Lactobacillus and Bifidobacterium, can influence the production of other key neurotransmitters like GABA (the main inhibitory, or calming, neurotransmitter).
The Leaky Gut and Systemic Inflammation Link
A crucial, often overlooked aspect is inflammation. When dysbiosis occurs, the protective mucus layer thins, and the tight junctions between the gut lining cells loosen, leading to increased intestinal permeability, commonly known as “leaky gut.”
This allows substances like lipopolysaccharides (LPS)—toxins released from the cell walls of certain Gram-negative bacteria—to “leak” into the bloodstream. This triggers a systemic immune response. When this chronic, low-grade inflammation crosses the blood-brain barrier (BBB), it can directly affect the brain, manifesting as brain fog, depression, anxiety, and even accelerating neurodegenerative processes. This mechanism underscores why targeting gut microbiome health is an essential strategy for mental resilience.
The Blueprint for Optimal Gut Microbiome Health: Actionable Strategies
Achieving and maintaining superb gut microbiome health requires a comprehensive strategy that goes beyond simply buying a bottle of probiotics. As an expert, I prioritize prebiotics—the food for your microbes—over propping them up with external sources.
Prebiotic Priority: Feeding Your Residents, Not Just Adding Tourists
The single most impactful dietary change you can make is to feed the beneficial bacteria already present in your gut with the fibers they need.
- Resistant Starch: This acts as a powerful fuel for butyrate producers. Sources include cooled white rice/potatoes (the cooling process increases resistant starch content), green bananas, and high-quality oat groats.
- Inulin and FOS (Fructans): Found in Jerusalem artichokes, chicory root, garlic, onions, and asparagus. These are potent bacterial feeders, but proceed slowly if you have a sensitive gut, as they can cause gas.
- Beta-Glucans: Found in oats and medicinal mushrooms. These support your microbes and possess immunomodulatory properties.
Dietary Diversity is King: The 30-Plant Rule
My most critical piece of advice is to prioritize diversity. Think of your gut as a biodiverse rainforest; the more varied the life, the more resilient the ecosystem.
- Expert Recommendation: Aim to consume 30 different types of plants per week. This includes fruits, vegetables, nuts, seeds, whole grains, herbs, and spices. Each plant source contains unique fibers and polyphenols (plant chemicals) that feed different specialized strains of bacteria.
- Supercharge Your Gut! The 30 Plant Foods Challenge. People who consumed 30 or more types of plants weekly had significantly more diverse and resilient microbiomes compared to those who ate fewer than 10. This report is compelling, data-driven evidence that supports a whole-foods approach to enhancing gut microbiome health.
Beyond the Plate: The Role of Exercise and Sleep
Your microbial community profoundly influences your lifestyle choices.
- Movement Matters: Regular exercise, especially moderate- to high-intensity training, has been shown to increase microbial diversity and, critically, increase the abundance of SCFA-producing bacteria. It’s not just your muscles that benefit—it’s your gut lining too.
The Sleep-Gut Damage Connection: Lack of quality sleep (less than 7 hours) significantly increases stress hormones and negatively impacts the integrity of the gut lining, potentially exacerbating “leaky gut.” Prioritizing deep, consistent sleep is a non-negotiable step for long-term gut microbiome health.
Ready to Transform Your Plate? Explore Our Full Nutrition Category Now! Click here
Expert Insight: Separating Microbiome Fact from Supplement Fiction
The supplement aisle is crowded, and the claims are often sensationalized. Based on my expertise, here is how you navigate the complexity and focus on interventions that truly support your gut microbiome health.
Probiotics: Targeted Therapy, Not a Shotgun Approach
Mass-market, cheap probiotics are often a “shotgun approach”—they contain common strains that may not colonize or survive the journey through the acidic stomach.
- Targeted Strains: True effectiveness comes from targeted strains. For instance, if you are seeking immune support, strains like Lactobacillus rhamnosus GG are well-researched. For managing acute mood issues, emerging evidence points towards specific psychobiotics like Bifidobacterium longum 1714 or Lactobacillus helveticus R0052. Always look for strain numbers.
- Soil-Based Organisms (SBOs): These are a unique class of probiotics that show great promise for resilience, but their effects require more research and should be managed with expert guidance.
H3: The Hidden Microbiome Killers to Avoid
To improve gut microbiome health, stopping the damage is often more important than adding supplements.
- Antibiotics: Use them wisely and only when necessary. A single course can wipe out microbial diversity for up to a year. Always follow an antibiotic course with aggressive prebiotic and targeted probiotic intervention.
- Common Food Additives: Emulsifiers such as Carboxymethylcellulose (CMC) and Polysorbate 80 (P80), commonly found in processed foods to improve texture and shelf life, have been shown in animal models to erode the protective mucus layer and promote dysbiosis. Read ingredient labels religiously.
- Chronic Stress: While not a chemical, chronic psychological stress floods the system with cortisol, changing the gut’s environment (pH, motility) and favoring the growth of less desirable microbes.
H3: The Future of Medicine: Fecal Microbiota Transplant (FMT)
For extreme cases, particularly recurrent Clostridium difficile infections, Fecal Microbiota Transplant (FMT) is a revolutionary treatment. This procedure, which involves transferring healthy fecal matter (and its microbes) from a screened donor to a patient, boasts a success rate of over 90% for C. difficile. While FMT is currently restricted to severe clinical settings, its success serves as powerful proof of concept: the microbiome truly is medicine.
Summary & Your Path to Astonishing Gut Microbiome Health
Your gut microbiome is not a passive passenger; it is an active, essential organ that contributes to your physical energy, mental clarity, and long-term disease resistance. My personal experience and professional insight confirm that investing in gut microbiome health yields exponential returns across all areas of wellness.
Three Simple Steps to Begin Your Microbiome Journey Today:
- Embrace Diversity: Commit to eating 30 unique plant foods per week. Focus on colorful produce, varied whole grains, and a rotating selection of nuts/seeds.
- Prioritize the Pillars: Ensure you are getting 7-9 hours of quality sleep and incorporating daily movement to support microbial signaling and reduce inflammation.
- Become a Fermentation Enthusiast: Incorporate small amounts of high-quality fermented foods (sauerkraut, kimchi, kefir—always check for live cultures) daily. This simple, traditional practice is a powerful tool for maintaining gut microbiome health.
The journey to astonishing health begins in your gut. Will you start listening to this hidden organ today?
Important Disclaimer
Please Note: The information presented in this article (“Meet Your Microbiome: The Hidden Organ That Shapes Your Health”) is for general informational and educational purposes only. This content is not intended to be, and must not be taken as, a substitute for professional medical advice, diagnosis, or treatment.
1. Not Medical Advice
- This article reflects the author’s expertise, research, and views on gut microbiome health.
- The information provided does not establish a doctor-patient relationship.
- Always seek the advice of your physician, registered dietitian, or other qualified health provider with any questions you may have regarding a medical condition, diagnosis, or treatment before making significant changes to your diet, supplements, or lifestyle.
2. Personal Responsibility
- Individual responses to dietary changes, prebiotics, or probiotics can vary widely.
- You assume full responsibility for your own health decisions. The author and publisher are not liable for any losses, injuries, or damages arising from the use or misuse of the information contained herein.
For more info



